What if a doctor could foresee health risks before they actually became a problem? If patients were able to get early warning signs for dangerous conditions?
Predictive analytics in healthcare makes it possible, completely changing the approach to early diagnostics and acute decision making.
Among the four main types of healthcare data analytics, predictive analytics currently has the highest potential to drive value.
Unlike descriptive or diagnostic analytics, it not only explains what has happened and why but helps anticipate what’s likely to happen next, using patterns in historical data.
For healthcare organizations, it’s a chance to shift from reactive care to a more proactive approach.
How Does Predictive Analytics Work in Healthcare?
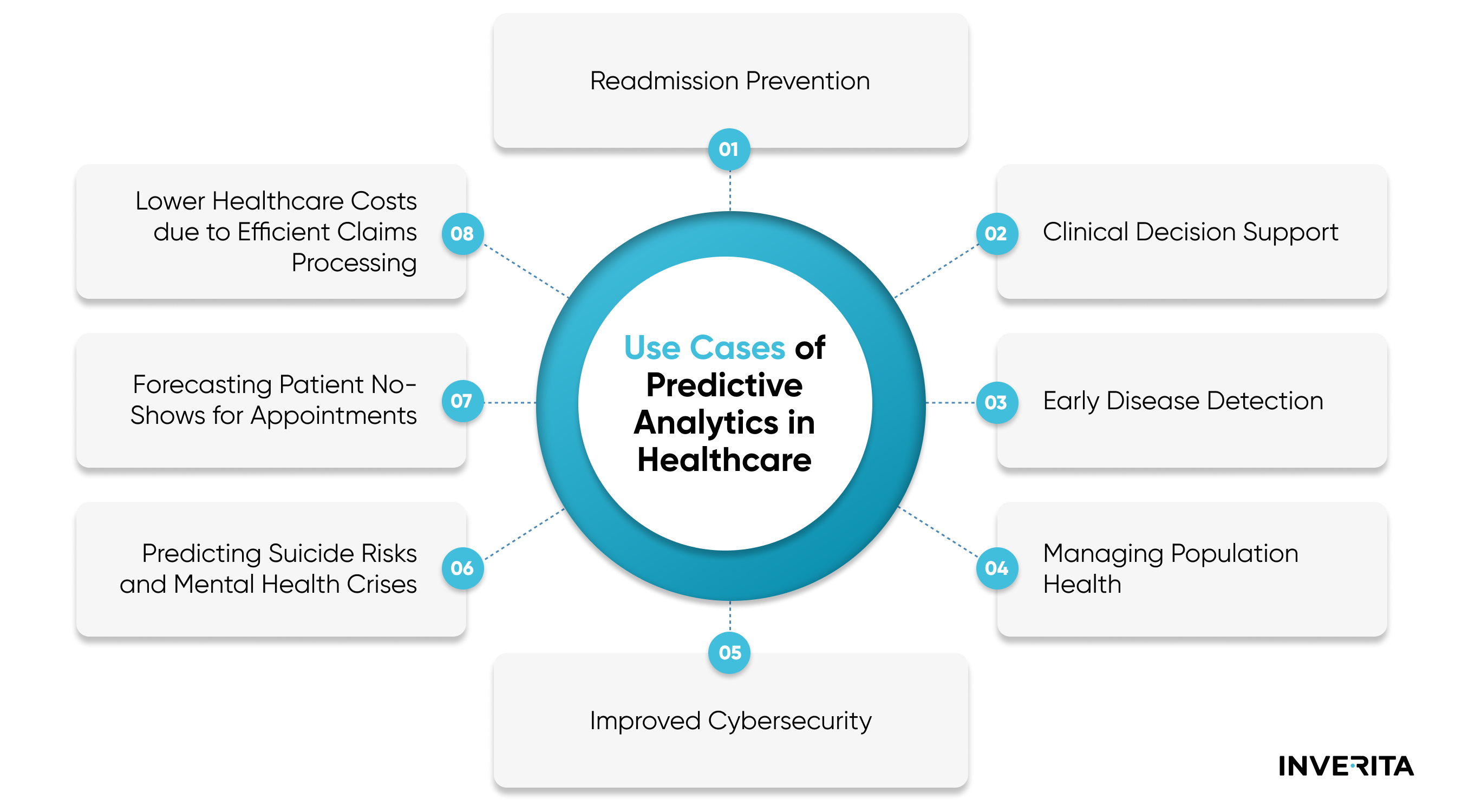
Predictive analytics for healthcare finds patterns and trends in high loads of analyzed healthcare data such as electronic health records, insurance claims, lab results, medical imaging, wearable devices, and even administrative paperwork.
With these insights, healthcare professionals can go beyond reacting to symptoms and start anticipating patient needs. For example:
- Which diseases is a patient at high risk of developing? (for example, diabetes, cardiovascular conditions, or certain cancers)
- How will they likely respond to different medications or treatment plans?
- Is a patient likely to miss their upcoming appointment? — helping to reduce no-show rates through targeted reminders or support.
- What’s the probability they’ll be readmitted within 30 days of discharge?
- Which patients may require ICU transfer based on early signs of deterioration?
- Can a patient’s condition be managed at home to avoid unnecessary ER visits?
Importance of Predictive Analytics for Healthcare Providers
Predictive analytics in healthcare is especially critical in emergency and intensive care, where patient outcomes are very dependent on quick reaction and personal decisions of care providers.
It helps spot risks early, personalize treatments, and prevent complications before they happen. By making sense of historical data, predictive models allow hospitals and doctors to act faster, use resources smartly, and deliver better care without driving up costs. It’s not just about faster diagnoses, it’s about making healthcare more proactive, efficient, and focused on what patients actually need.
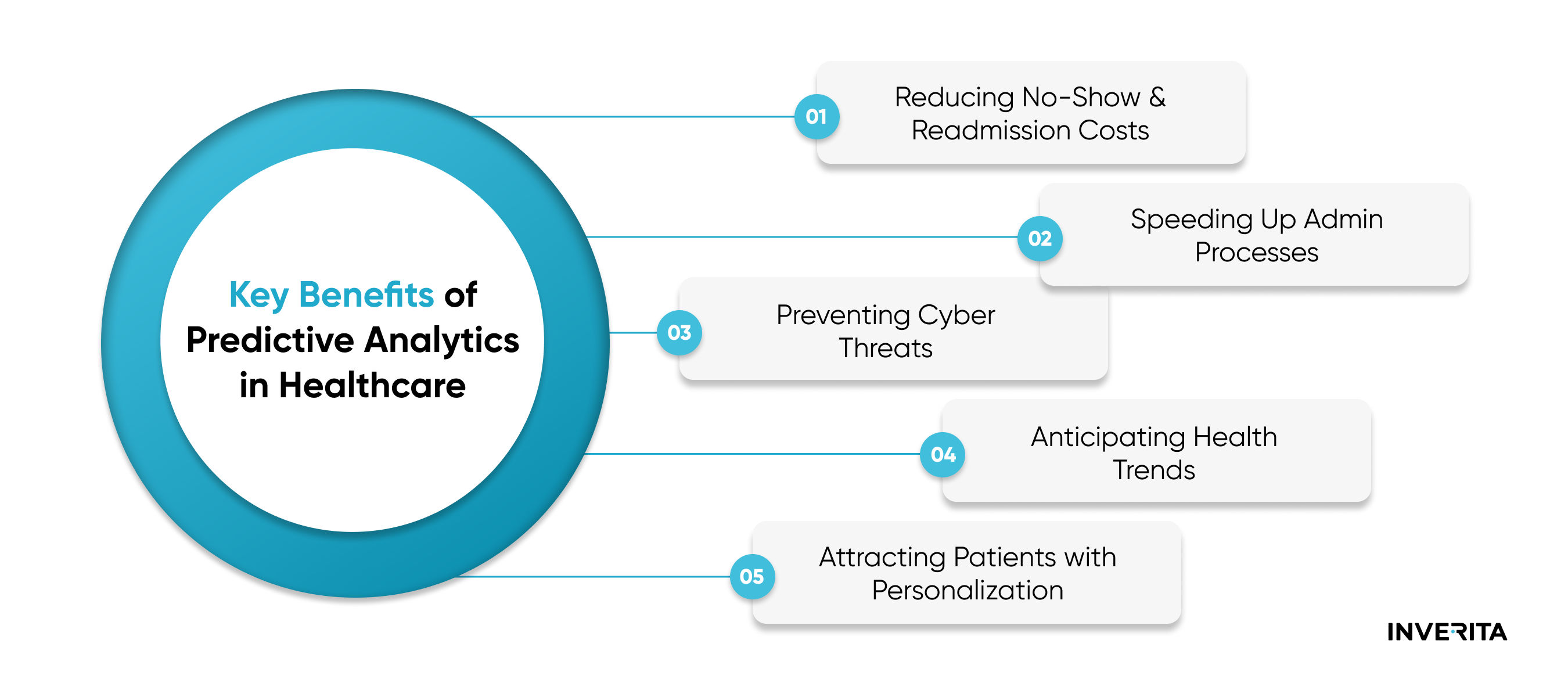
Key Benefits of Predictive Analytics in Healthcare
Predictive analytics is reshaping healthcare by offering new ways to improve patient outcomes, manage costs, and strengthen preventive care.
By using historical and real-time data, healthcare providers can detect risks earlier, make better-informed decisions, and deliver more personalized treatments.