Healthcare data creates a paradox: it needs to be kept private and secure due to its sensitive nature, which makes it challenging to share. However, not having secure access to this data when necessary can have serious, even fatal consequences.
Without data interoperability healthcare providers can’t have a complete understanding of patient’s or the population’s health needs.
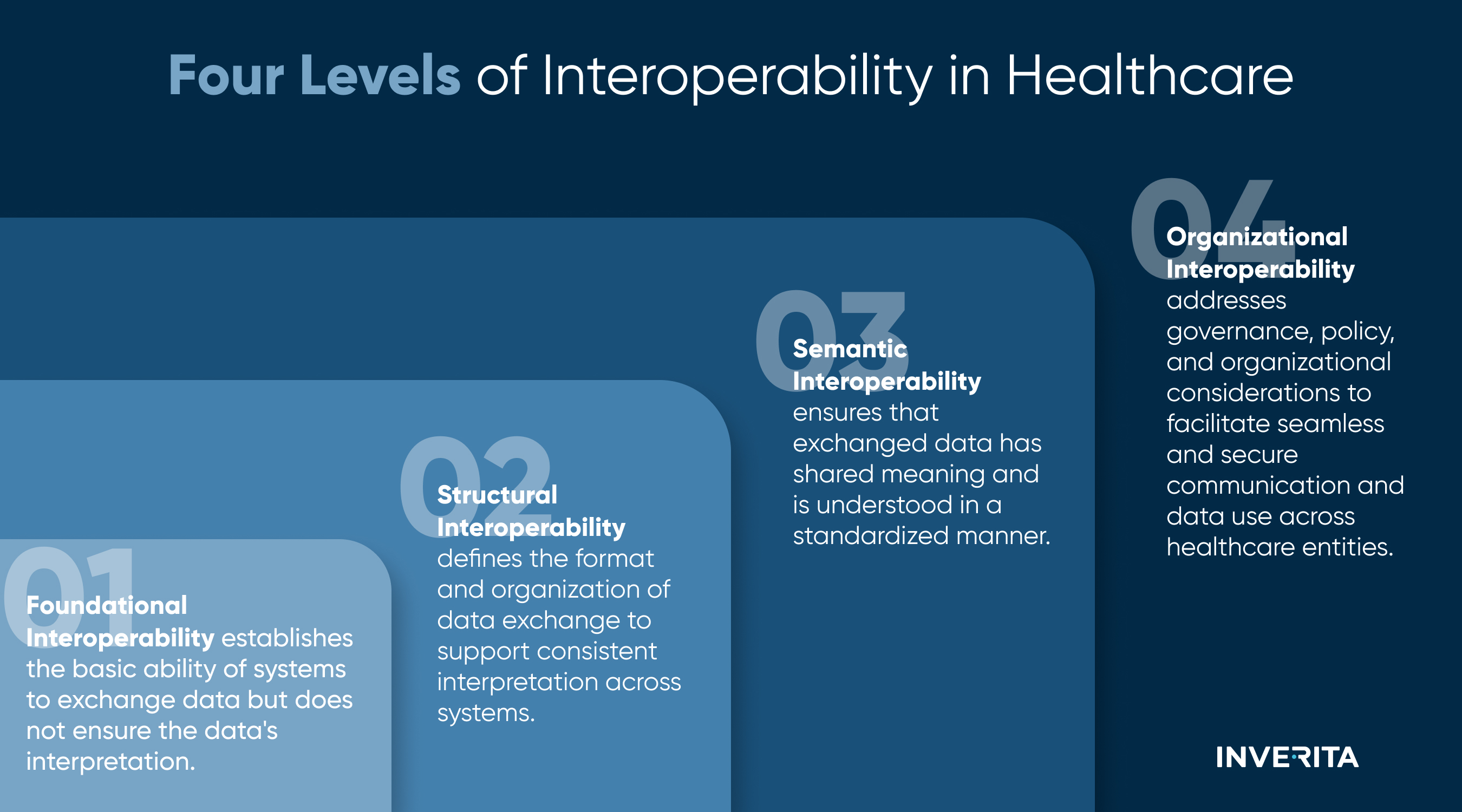
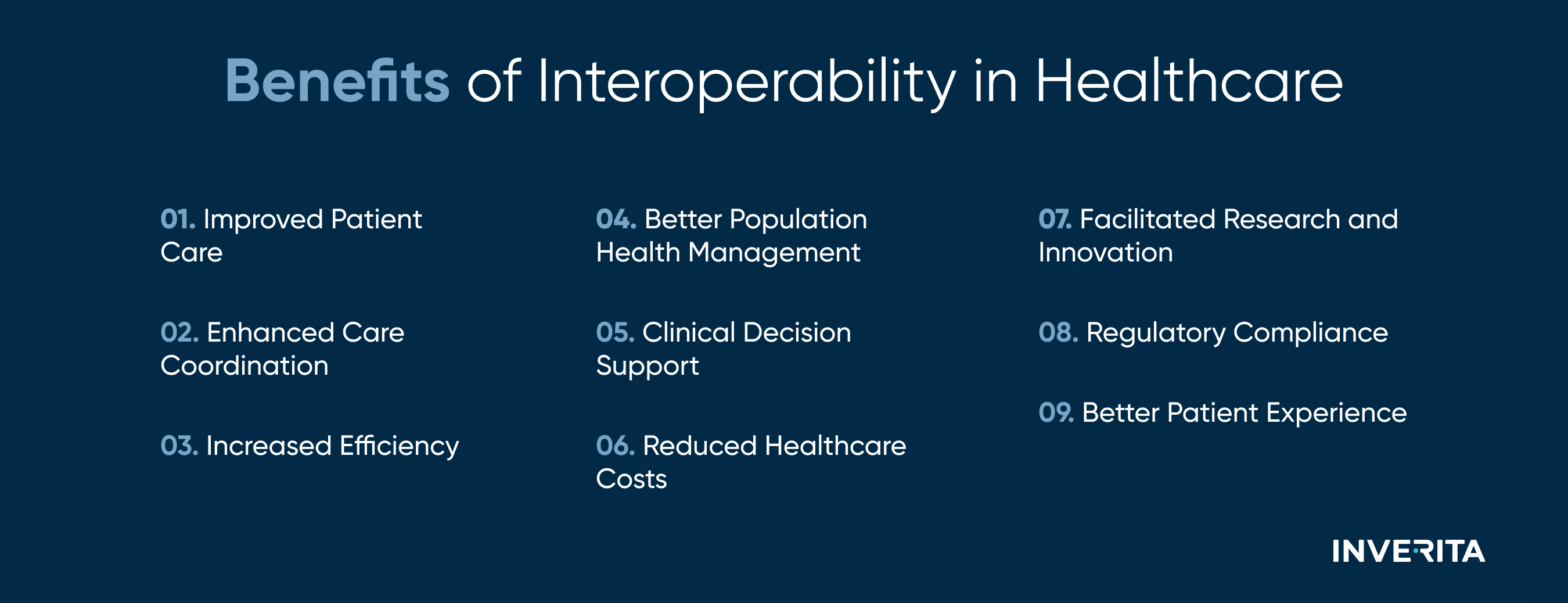
What is healthcare interoperability, the four types of interoperability in healthcare, current challenges it faces, and the benefits of data interoperability healthcare providers can get - in today’s blog.
What is Interoperability in Healthcare?
So, what is interoperability in healthcare?
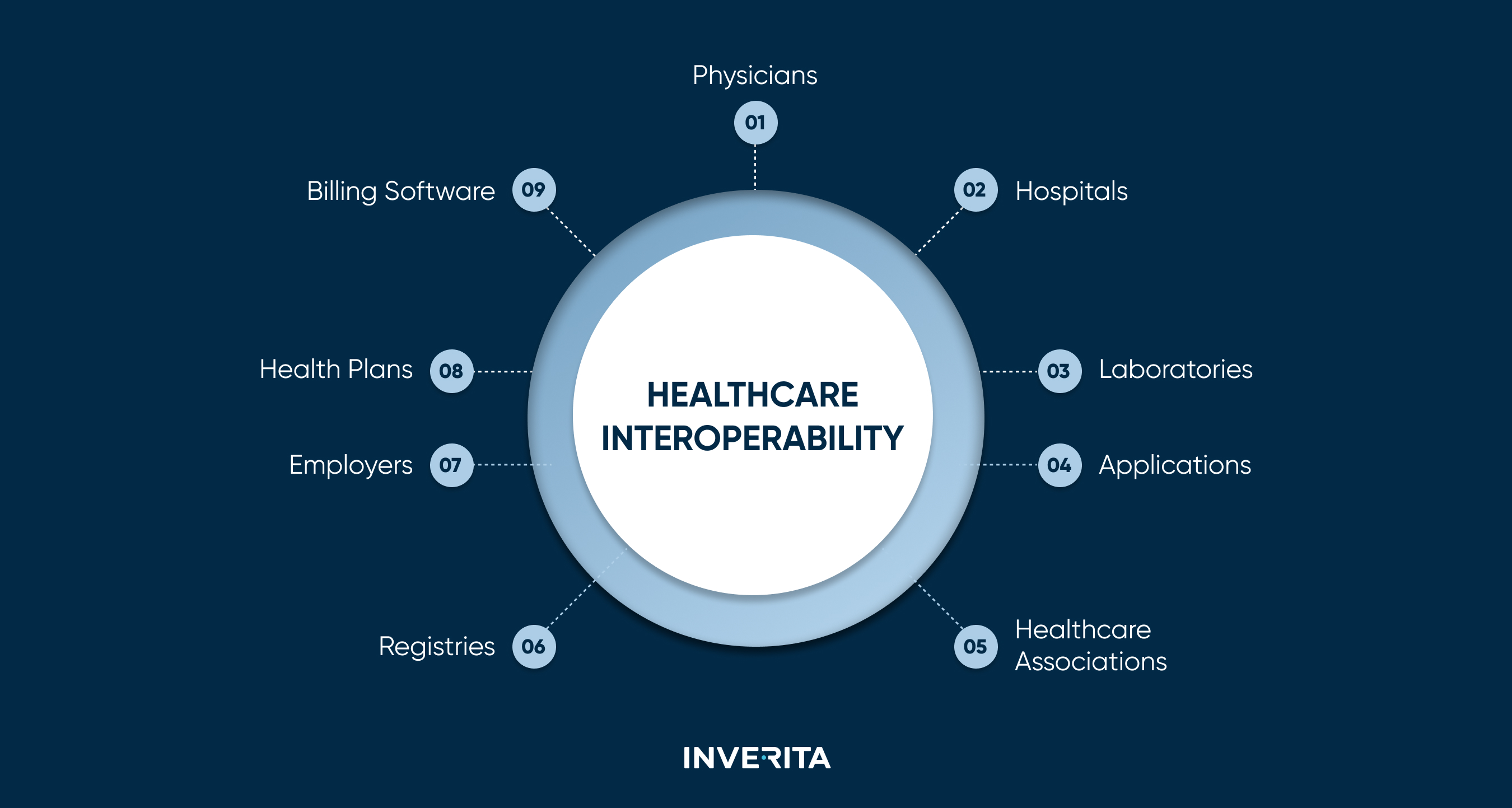
Healthcare Information and Management System Society (HIMSS) defines healthcare interoperability as “the ability of various information systems, devices, and applications to access, exchange, integrate, and use data together in a coordinated way. This coordination occurs within and across regional, national, and organizational boundaries to ensure the timely and seamless transfer of information, ultimately optimizing the health of individuals and populations worldwide”.
In very simple words, data interoperability in healthcare means that different medical systems and gadgets can talk to each other and share information without any hassle. This makes it easier for healthcare professionals and hospitals to get the right patient info when they need it, leading to better care and improving patient outcomes.
Let’s see it in the example.
Imagine a patient visiting your clinic after recently undergoing diagnostic imaging at a specialized facility. With interoperable systems in place, accessing the patient’s imaging results becomes seamless. This enables you to quickly review the images during the consultation, facilitating a more informed discussion about the patient's condition and treatment plan. Subsequently, the imaging results are effortlessly shared with other healthcare providers within your clinic for further assessment or treatment care coordination.
Now, suppose the patient requires a specific medication that was prescribed during a recent hospitalization. With interoperable systems, retrieving the patient's medication history from the hospital's electronic medical records becomes straightforward. This ensures that you have access to vital information about the patient's past medications, enabling you to make informed decisions about their current treatment regimen.
Following the consultation, the patient's treatment plan may involve a combination of medications and therapies. Interoperable systems streamline the coordination of care by enabling seamless communication between different medical professionals involved in the patient's treatment. This ensures that everyone has access to the latest information, promoting continuity of care and patient safety.